Mucus in Stool: Causes, Symptoms, Diagnosis & Treatment Options
Mucus in Stool: Causes, Symptoms, Diagnosis & Treatment Options Adequate fluid intake is essential, especially if you’re experiencing diarrhea, to prevent dehydration and support normal digestive function. Stress Management Since stress can significantly impact digestive health, techniques like meditation, yoga, deep breathing exercises, and regular physical activity can help reduce symptoms. Expert Care at Laxmi Hospital Kochi When digestive symptoms persist or cause concern, seeking expert medical evaluation is crucial for accurate diagnosis and effective treatment. Laxmi Hospital Kochi offers comprehensive gastroenterology services with experienced specialists who can thoroughly evaluate and treat conditions causing mucus in stool. The hospital is equipped with advanced diagnostic facilities including modern endoscopy units, state-of-the-art imaging technology, and comprehensive laboratory services. Whether you need routine diagnostic procedures, management of chronic digestive conditions, or specialized treatment for complex gastrointestinal disorders, Laxmi Hospital Kochi provides patient-centered care with a multidisciplinary approach. The gastroenterology team at Laxmi Hospital Kochi works closely with other specialists to ensure that all aspects of your digestive health are addressed. From initial consultation through diagnosis and treatment, the hospital’s commitment to quality care and patient comfort makes it a trusted choice for addressing digestive health concerns in the Kochi region. Prevention and Maintaining Digestive Health While not all causes of mucus in stool can be prevented, you can take steps to maintain optimal digestive health: Practice good hand hygiene, especially before eating and after using the bathroom Eat a balanced diet rich in fiber from fruits, vegetables, and whole grains Stay well-hydrated by drinking adequate water throughout the day Exercise regularly to promote healthy digestion Manage stress through relaxation techniques Avoid foods that trigger symptoms Don’t ignore persistent digestive symptoms Get age-appropriate colorectal cancer screenings Moving Forward Discovering mucus in your stool doesn’t necessarily indicate a serious problem, but it’s your body’s way of signaling that something has changed in your digestive system. By paying attention to associated symptoms and seeking appropriate medical care when needed, you can identify and address the underlying cause effectively. Remember that digestive health is an essential component of overall wellbeing. Don’t hesitate to discuss concerns with your healthcare provider—early evaluation and treatment typically lead to better outcomes and faster symptom resolution. With proper diagnosis and management, most conditions causing excess mucus in stool can be effectively treated, allowing you to return to normal digestive function and improved quality of life.
Sinus Infection (Sinusitis): Causes, Symptoms & Prevention Tips
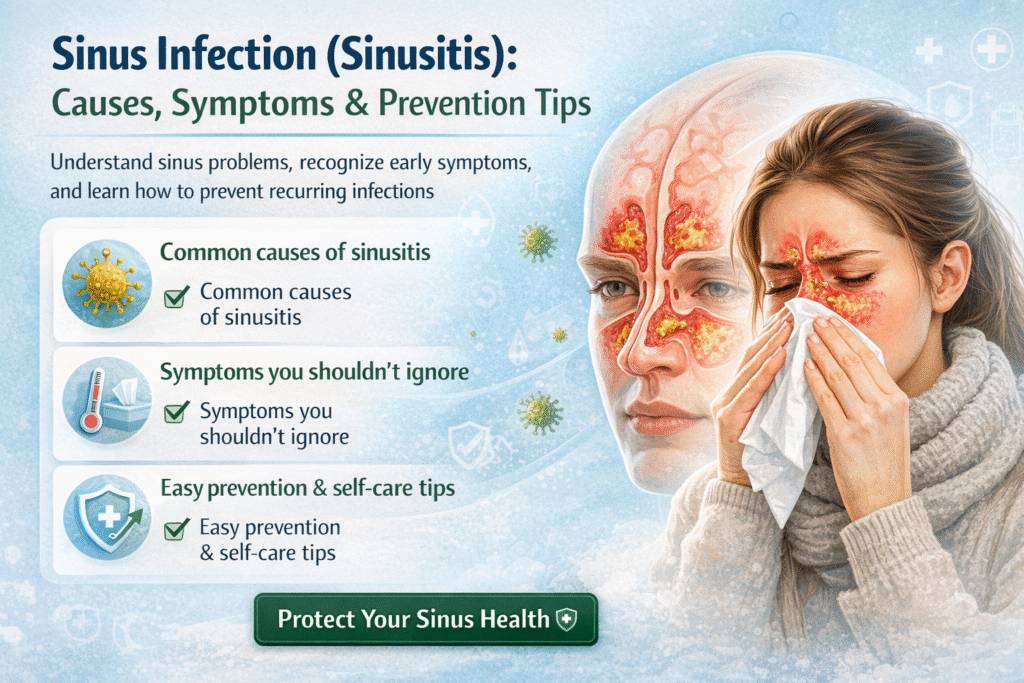
Sinus Infection (Sinusitis): Causes, Symptoms & Prevention Tips Sinus infections, medically known as sinusitis, affect millions of people worldwide each year. If you’ve ever experienced the throbbing facial pain, persistent nasal congestion, and overwhelming fatigue that accompanies a sinus infection, you know just how disruptive this condition can be to daily life. Understanding the causes, recognizing the symptoms, and knowing how to prevent sinusitis can help you manage this common but uncomfortable condition more effectively. What is Sinusitis? Sinusitis is an inflammation or swelling of the tissue lining the sinuses. Your sinuses are hollow cavities within the bones surrounding your nose, including your forehead, cheeks, and between your eyes. When healthy, these air-filled spaces are lined with a thin layer of mucus that traps dust, germs, and other particles from the air you breathe. Normally, mucus drains out of the sinuses and into the nose. However, when the sinuses become blocked and filled with fluid, bacteria, viruses, or fungi can grow and cause an infection. This blockage and inflammation is what we call sinusitis. Types of Sinusitis Sinusitis is classified based on how long it lasts: Acute Sinusitis typically lasts less than four weeks and often follows a cold or upper respiratory infection. This is the most common type of sinusitis. Subacute Sinusitis lasts between four and twelve weeks and represents a transition between acute and chronic forms. Chronic Sinusitis persists for twelve weeks or longer despite treatment attempts. This form can significantly impact quality of life and may require more aggressive management. Recurrent Sinusitis occurs when someone experiences several acute episodes within a year, typically four or more instances with symptom-free periods in between. Common Causes of Sinus Infections Understanding what triggers sinusitis can help you take preventive measures and seek appropriate treatment. Viral Infections The most common cause of acute sinusitis is a viral infection, often the common cold. When you have a cold, the viral infection causes inflammation and swelling in the nasal passages, which can block the sinus openings and prevent normal drainage. Bacterial Infections Sometimes a viral sinus infection can develop into a bacterial infection. This typically happens when symptoms persist beyond 10 days or worsen after initially improving. Bacteria such as Streptococcus pneumoniae and Haemophilus influenzae commonly cause bacterial sinusitis. Allergies Allergic reactions to pollen, dust mites, pet dander, or mold can cause inflammation in the nasal passages and sinuses. People with allergic rhinitis (hay fever) are more susceptible to developing sinusitis because the constant inflammation can interfere with proper sinus drainage. Nasal Polyps These benign growths in the nasal passages or sinuses can block sinus openings, preventing proper drainage and leading to infection. Deviated Septum A deviated nasal septum—when the wall between the nostrils is crooked or off-center—can restrict sinus drainage and increase the likelihood of infections. Other Contributing Factors Additional factors that can increase your risk of developing sinusitis include: Smoking or exposure to secondhand smoke Air pollution and environmental irritants Weakened immune system Respiratory tract infections Dental infections that spread to the sinuses Swimming or diving, which can push water into the sinuses Changes in air pressure during flying or scuba diving Overuse of nasal decongestant sprays Recognizing the Symptoms Sinus infection symptoms can vary in intensity and may overlap with other conditions, making proper diagnosis important. Primary Symptoms Facial pain and pressure are hallmark symptoms of sinusitis. You may feel a dull, aching sensation or pressure around your eyes, cheeks, nose, or forehead. This discomfort often worsens when you bend forward or lie down. Nasal congestion makes breathing through your nose difficult. The blocked feeling is caused by inflamed nasal passages and excess mucus production. Thick, discolored nasal discharge is another key indicator. The mucus may be yellow, green, or cloudy, and you may notice it draining down the back of your throat, a condition called postnasal drip. Reduced sense of smell and taste occurs because inflammation blocks odor receptors in your nose. Many people find food tastes bland during a sinus infection. Additional Symptoms Beyond the primary symptoms, sinusitis can cause: Headache, often concentrated in the forehead or around the eyes Ear pressure or fullness Aching in your upper jaw and teeth Cough that may worsen at night Sore throat from postnasal drip Bad breath (halitosis) Fatigue and general feeling of being unwell Fever, particularly with bacterial infections When to See a Doctor While many sinus infections resolve on their own, you should seek medical attention if: Symptoms last more than 10 days without improvement Symptoms are severe or unusual You experience high fever (above 102°F or 39°C) You’ve had multiple sinus infections in the past year Symptoms initially improve but then worsen You experience vision changes, severe headache, or neck stiffness Effective Prevention Tips While you can’t prevent all sinus infections, you can significantly reduce your risk by following these evidence-based strategies. Practice Good Hygiene Wash your hands frequently with soap and water, especially during cold and flu season. Avoid touching your face, particularly your nose and eyes, which can introduce germs into your sinuses. Stay away from people who have colds or other respiratory infections when possible. Stay Hydrated Drinking plenty of fluids helps thin mucus, making it easier to drain from your sinuses. Aim for at least eight glasses of water daily. Warm liquids like herbal tea, broth, or hot water with lemon can be especially soothing. Use a Humidifier Dry air can irritate your nasal passages and sinuses. Using a humidifier, especially during winter months or in dry climates, adds moisture to the air and helps keep your nasal passages moist. Clean your humidifier regularly to prevent mold and bacteria growth. Manage Allergies If you have allergies, work with your healthcare provider to keep them under control. This might include using antihistamines, nasal corticosteroid sprays, or allergy shots. Reducing allergen exposure by using air purifiers, washing bedding regularly, and keeping windows closed during high pollen seasons can help. Practice Nasal Irrigation Regular nasal irrigation with a saline solution can flush out allergens, irritants, and
Top Lifestyle Changes to Slow Down Heart Ageing & Improve Heart Health
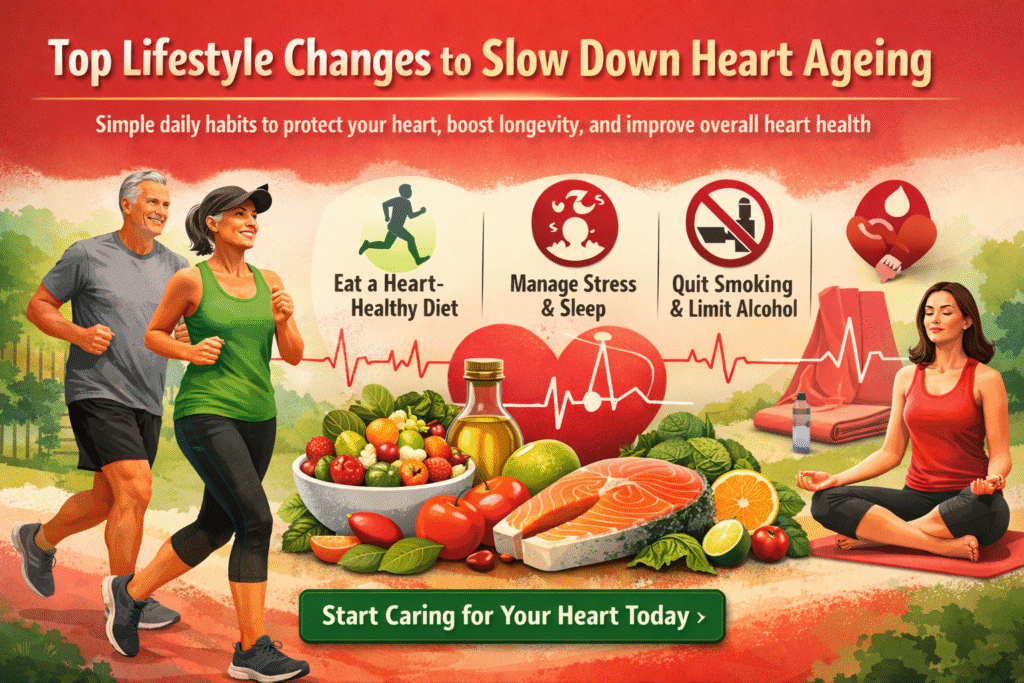
Top Lifestyle Changes to Slow Down Heart Ageing & Improve Heart Health Your heart is your body’s most tireless worker, beating approximately 100,000 times each day, pumping blood through 60,000 miles of blood vessels. Yet despite its remarkable endurance, the heart is vulnerable to the effects of aging and lifestyle choices. The good news is that heart aging isn’t entirely predetermined by genetics—your daily habits play a crucial role in determining your cardiovascular health as you age. Understanding Heart Aging Before diving into lifestyle changes, it’s important to understand what happens to your heart as it ages. With time, the heart muscle can become slightly thickened, the arteries may stiffen, and the efficiency of blood pumping can decrease. However, research shows that many of these changes can be slowed, prevented, or even reversed through conscious lifestyle modifications. 1. Embrace Regular Physical Activity Exercise is perhaps the most powerful tool in your heart-health arsenal. Regular physical activity strengthens your heart muscle, improves circulation, helps maintain healthy blood pressure, and reduces inflammation throughout your body. Aim for a balanced approach: Combine aerobic exercises like brisk walking, swimming, or cycling with strength training exercises at least twice a week. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous activity weekly. Even if you’ve been sedentary for years, it’s never too late to start—studies show that beginning an exercise program in middle age can significantly reduce cardiovascular risk. Start slowly if you’re new to exercise. A 10-minute walk after meals can be a perfect beginning. Gradually increase duration and intensity as your fitness improves. Remember, consistency matters more than intensity when it comes to long-term heart health. 2. Adopt a Heart-Healthy Diet What you eat directly impacts your cardiovascular system. A heart-healthy diet can reduce cholesterol levels, lower blood pressure, decrease inflammation, and help maintain a healthy weight. The Mediterranean diet has emerged as one of the best eating patterns for heart health. This approach emphasizes whole grains, fruits, vegetables, legumes, nuts, olive oil, and fish while limiting red meat and processed foods. Studies show that people following this diet have significantly lower rates of heart disease. Key dietary principles include: Fill half your plate with colorful vegetables and fruits Choose whole grains over refined carbohydrates Include healthy fats from sources like avocados, nuts, seeds, and fatty fish Limit saturated fats found in red meat and full-fat dairy products Reduce sodium intake to help control blood pressure Minimize added sugars and processed foods Omega-3 fatty acids, found abundantly in fatty fish like salmon, mackerel, and sardines, have powerful anti-inflammatory properties and can help reduce triglycerides and improve arterial health. If you don’t eat fish, consider walnuts, flaxseeds, or consult your doctor about supplements. 3. Maintain a Healthy Weight Excess body weight, particularly around the abdomen, puts additional strain on your heart and increases risk factors like high blood pressure, diabetes, and high cholesterol. Even modest weight loss of 5-10% of your body weight can produce significant improvements in heart health markers. Focus on sustainable changes rather than crash diets. Combine mindful eating with regular physical activity for lasting results. Remember that where you carry weight matters—visceral fat around the abdomen is particularly harmful to cardiovascular health. 4. Manage Stress Effectively Chronic stress triggers the release of stress hormones like cortisol and adrenaline, which can raise blood pressure, increase heart rate, and contribute to inflammation. Over time, unmanaged stress accelerates heart aging. Develop healthy stress management techniques: Practice mindfulness meditation or deep breathing exercises Engage in yoga or tai chi Maintain strong social connections Pursue hobbies and activities you enjoy Consider professional counseling if stress feels overwhelming Even 10-15 minutes of daily meditation or relaxation practice can make a meaningful difference in your cardiovascular health. 5. Prioritize Quality Sleep Sleep is when your body repairs and regenerates, including your cardiovascular system. During deep sleep, your heart rate and blood pressure drop, giving your heart a much-needed rest. Chronic sleep deprivation increases the risk of high blood pressure, obesity, diabetes, and heart disease. Aim for 7-9 hours of quality sleep each night. Establish a consistent sleep schedule, create a relaxing bedtime routine, keep your bedroom cool and dark, and limit screen time before bed. If you snore loudly or experience daytime fatigue despite adequate sleep time, talk to your doctor about sleep apnea, which significantly increases heart disease risk. 6. Quit Smoking and Limit Alcohol If you smoke, quitting is the single most important step you can take for your heart health. Smoking damages blood vessel walls, reduces oxygen in your blood, raises blood pressure, and increases clot formation. The good news is that your heart begins to heal almost immediately after quitting—within just one year, your risk of heart disease drops to about half that of a smoker. Regarding alcohol, moderation is key. While some studies suggest small amounts of alcohol may have cardiovascular benefits, excessive drinking clearly harms the heart. If you choose to drink, limit intake to no more than one drink per day for women and two for men. 7. Monitor Your Numbers Regular health screenings help catch potential problems early. Work with your healthcare provider to monitor: Blood pressure (aim for below 120/80 mmHg) Cholesterol levels (including LDL, HDL, and triglycerides) Blood sugar levels (to detect prediabetes or diabetes) Body mass index (BMI) and waist circumference Understanding your numbers empowers you to make informed decisions about your health and track the effectiveness of your lifestyle changes. 8. Stay Hydrated Proper hydration helps your heart pump blood more easily and helps your muscles work efficiently. Dehydration can strain your cardiovascular system. Aim for 8-10 glasses of water daily, adjusting for activity level and climate. 9. Build Strong Social Connections Loneliness and social isolation increase heart disease risk. Meaningful relationships and social engagement contribute to lower stress levels, better health behaviors, and improved overall wellbeing. Make time for friends and family, join community groups, or volunteer—your heart will benefit. Expert Care at Laxmi
First 5 Minutes of a Stroke: Signs You Should Never Ignore
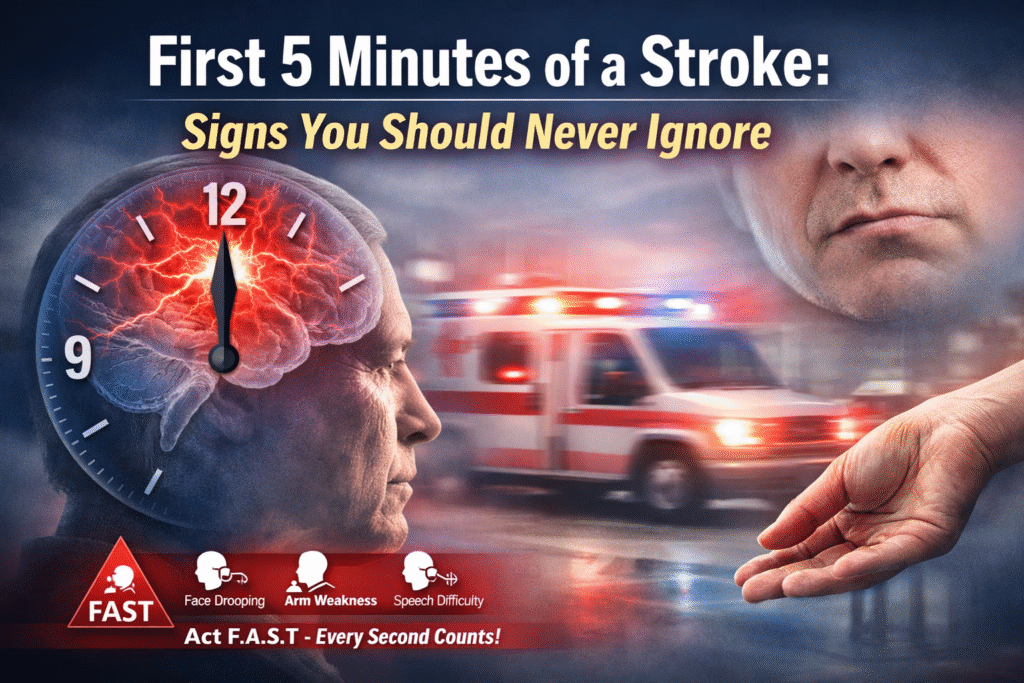
First 5 Minutes of a Stroke: Signs You Should Never Ignore Every second counts when it comes to stroke. The first few minutes after stroke symptoms appear are absolutely critical, and recognizing the warning signs immediately can mean the difference between full recovery and permanent disability—or even life and death. Understanding what happens in those crucial first five minutes and knowing how to respond can save your life or the life of someone you love. What Happens During a Stroke? A stroke occurs when blood flow to a part of the brain is interrupted or reduced, preventing brain tissue from getting the oxygen and nutrients it needs. Brain cells begin to die within minutes, making stroke a true medical emergency. There are two main types of stroke: ischemic strokes, caused by blocked blood vessels, account for about 87% of all strokes, while hemorrhagic strokes result from bleeding in the brain. The brain is an incredibly delicate organ, and when deprived of oxygen-rich blood, it begins to suffer damage almost immediately. This is why the medical community emphasizes that “time is brain”—every minute that passes without treatment means more brain cells are lost forever. Research shows that for every minute a stroke goes untreated, the average patient loses approximately 1.9 million neurons, which underscores the urgency of immediate action. The Critical First Five Minutes: What You Must Know The first five minutes after stroke symptoms begin represent your most valuable window of opportunity. During this time, your actions or the actions of those around you will set the course for treatment and recovery. Here’s what makes these moments so crucial: Immediate Recognition Saves Lives: The faster stroke symptoms are identified, the sooner emergency medical services can be activated. This early response is essential because stroke treatments are time-sensitive. For instance, the clot-busting medication tPA (tissue plasminogen activator) must typically be administered within 4.5 hours of symptom onset, and ideally much sooner for maximum effectiveness. Brain Damage Accumulates Rapidly: With each passing minute, more brain tissue dies. The damage that occurs in the first five minutes may be minimal compared to what happens if treatment is delayed by hours, but the clock is ticking from the very first second. Early intervention can minimize this damage significantly. The Window for Treatment is Narrow: While some stroke treatments can be performed beyond the first few hours, the best outcomes occur when treatment begins within the first 60 minutes, often called the “golden hour.” Those first five minutes of recognition and response are what make reaching medical care within that golden hour possible. The FAST Test: Your Lifesaving Tool The FAST acronym is a simple, memorable way to identify the most common stroke symptoms and know when to call emergency services. Let’s break down each component: F – Face Drooping: Ask the person to smile. Does one side of the face droop or feel numb? Is the smile uneven or lopsided? Facial drooping typically affects one side of the face and occurs because the stroke has damaged the area of the brain that controls facial muscles. The person may not be aware that their face looks different, so it’s important to observe this yourself or have them look in a mirror. A – Arm Weakness: Ask the person to raise both arms. Does one arm drift downward or feel weak or numb? Have them close their eyes and hold both arms straight out in front of them. If one arm begins to fall, this indicates weakness on that side of the body. The person may also be unable to raise one arm at all. S – Speech Difficulty: Ask the person to repeat a simple sentence like “The sky is blue.” Is their speech slurred or strange? Do they have trouble speaking or understanding you? Speech problems during a stroke can manifest in several ways: slurred speech, using wrong words, being unable to speak at all, or difficulty understanding what others are saying. T – Time to Call Emergency Services: If you observe any of these signs, even if they go away, call emergency services immediately. Note the time when symptoms first appeared, as this information is crucial for treatment decisions at the hospital. Additional Warning Signs You Shouldn’t Ignore While FAST covers the most common symptoms, strokes can present in other ways. Be alert for these additional warning signs: Sudden Confusion or Trouble Understanding: The person may seem disoriented, confused about where they are, or unable to follow simple instructions. They might not recognize familiar people or places. Sudden Vision Problems: This can include trouble seeing in one or both eyes, blurred vision, blackened vision, or double vision. The person might complain that things look strange or that they can’t see properly on one side. Sudden Severe Headache: An intense headache that comes on suddenly without a known cause can indicate a hemorrhagic stroke. This is often described as the worst headache of one’s life and may be accompanied by vomiting, altered consciousness, or neck stiffness. Sudden Trouble Walking: Loss of balance, dizziness, or lack of coordination can signal a stroke, especially when combined with other symptoms. The person may stumble, feel dizzy, or be unable to walk in a straight line. Sudden Numbness: Numbness or weakness, particularly on one side of the body, affecting the face, arm, or leg. This can feel like a “pins and needles” sensation or complete loss of feeling. What to Do in the First Five Minutes If you suspect someone is having a stroke, here’s exactly what you should do: Call Emergency Services Immediately: Don’t wait to see if symptoms improve. Don’t call a family member first or try to drive to the hospital yourself. Call for an ambulance right away. Paramedics can begin life-saving treatment on the way to the hospital and can alert the emergency department so the stroke team is ready when you arrive. Note the Time: Write down or remember when the symptoms first began. This information is critical for determining which treatments
