First 5 Minutes of a Stroke: Signs You Should Never Ignore
Every second counts when it comes to stroke. The first few minutes after stroke symptoms appear are absolutely critical, and recognizing the warning signs immediately can mean the difference between full recovery and permanent disability—or even life and death. Understanding what happens in those crucial first five minutes and knowing how to respond can save your life or the life of someone you love.
What Happens During a Stroke?
A stroke occurs when blood flow to a part of the brain is interrupted or reduced, preventing brain tissue from getting the oxygen and nutrients it needs. Brain cells begin to die within minutes, making stroke a true medical emergency. There are two main types of stroke: ischemic strokes, caused by blocked blood vessels, account for about 87% of all strokes, while hemorrhagic strokes result from bleeding in the brain.
The brain is an incredibly delicate organ, and when deprived of oxygen-rich blood, it begins to suffer damage almost immediately. This is why the medical community emphasizes that “time is brain”—every minute that passes without treatment means more brain cells are lost forever. Research shows that for every minute a stroke goes untreated, the average patient loses approximately 1.9 million neurons, which underscores the urgency of immediate action.
The Critical First Five Minutes: What You Must Know
The first five minutes after stroke symptoms begin represent your most valuable window of opportunity. During this time, your actions or the actions of those around you will set the course for treatment and recovery. Here’s what makes these moments so crucial:
Immediate Recognition Saves Lives: The faster stroke symptoms are identified, the sooner emergency medical services can be activated. This early response is essential because stroke treatments are time-sensitive. For instance, the clot-busting medication tPA (tissue plasminogen activator) must typically be administered within 4.5 hours of symptom onset, and ideally much sooner for maximum effectiveness.
Brain Damage Accumulates Rapidly: With each passing minute, more brain tissue dies. The damage that occurs in the first five minutes may be minimal compared to what happens if treatment is delayed by hours, but the clock is ticking from the very first second. Early intervention can minimize this damage significantly.
The Window for Treatment is Narrow: While some stroke treatments can be performed beyond the first few hours, the best outcomes occur when treatment begins within the first 60 minutes, often called the “golden hour.” Those first five minutes of recognition and response are what make reaching medical care within that golden hour possible.
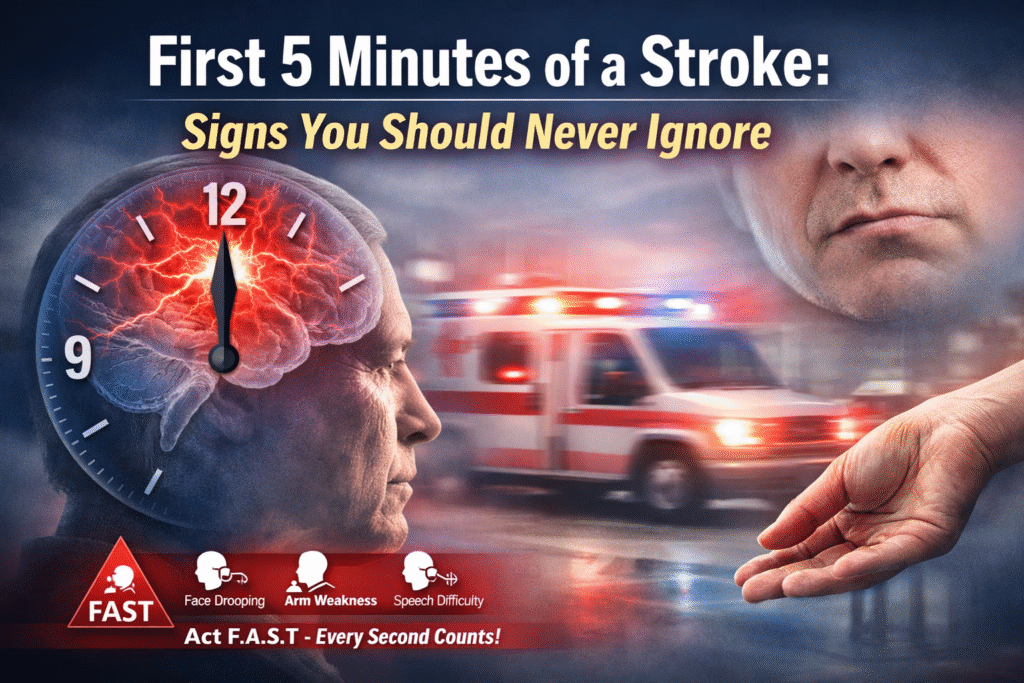
The FAST Test: Your Lifesaving Tool
The FAST acronym is a simple, memorable way to identify the most common stroke symptoms and know when to call emergency services. Let’s break down each component:
F – Face Drooping: Ask the person to smile. Does one side of the face droop or feel numb? Is the smile uneven or lopsided? Facial drooping typically affects one side of the face and occurs because the stroke has damaged the area of the brain that controls facial muscles. The person may not be aware that their face looks different, so it’s important to observe this yourself or have them look in a mirror.
A – Arm Weakness: Ask the person to raise both arms. Does one arm drift downward or feel weak or numb? Have them close their eyes and hold both arms straight out in front of them. If one arm begins to fall, this indicates weakness on that side of the body. The person may also be unable to raise one arm at all.
S – Speech Difficulty: Ask the person to repeat a simple sentence like “The sky is blue.” Is their speech slurred or strange? Do they have trouble speaking or understanding you? Speech problems during a stroke can manifest in several ways: slurred speech, using wrong words, being unable to speak at all, or difficulty understanding what others are saying.
T – Time to Call Emergency Services: If you observe any of these signs, even if they go away, call emergency services immediately. Note the time when symptoms first appeared, as this information is crucial for treatment decisions at the hospital.
Additional Warning Signs You Shouldn’t Ignore
While FAST covers the most common symptoms, strokes can present in other ways. Be alert for these additional warning signs:
Sudden Confusion or Trouble Understanding: The person may seem disoriented, confused about where they are, or unable to follow simple instructions. They might not recognize familiar people or places.
Sudden Vision Problems: This can include trouble seeing in one or both eyes, blurred vision, blackened vision, or double vision. The person might complain that things look strange or that they can’t see properly on one side.
Sudden Severe Headache: An intense headache that comes on suddenly without a known cause can indicate a hemorrhagic stroke. This is often described as the worst headache of one’s life and may be accompanied by vomiting, altered consciousness, or neck stiffness.
Sudden Trouble Walking: Loss of balance, dizziness, or lack of coordination can signal a stroke, especially when combined with other symptoms. The person may stumble, feel dizzy, or be unable to walk in a straight line.
Sudden Numbness: Numbness or weakness, particularly on one side of the body, affecting the face, arm, or leg. This can feel like a “pins and needles” sensation or complete loss of feeling.
What to Do in the First Five Minutes
If you suspect someone is having a stroke, here’s exactly what you should do:
Call Emergency Services Immediately: Don’t wait to see if symptoms improve. Don’t call a family member first or try to drive to the hospital yourself. Call for an ambulance right away. Paramedics can begin life-saving treatment on the way to the hospital and can alert the emergency department so the stroke team is ready when you arrive.
Note the Time: Write down or remember when the symptoms first began. This information is critical for determining which treatments the person is eligible to receive. If the person woke up with symptoms, the last time they were known to be normal is considered the onset time.
Keep the Person Calm and Comfortable: Have them lie down with their head slightly elevated. Loosen any tight clothing around the neck. Don’t give them anything to eat or drink, as stroke can impair their ability to swallow safely.
Don’t Give Medication: Even if you have aspirin, don’t give it to someone experiencing stroke symptoms. While aspirin is sometimes used in stroke treatment, it can be dangerous in hemorrhagic strokes, and only medical professionals should make this determination.
Stay with the Person: Monitor their condition closely. If they become unconscious, check their breathing and be prepared to perform CPR if you’re trained to do so.
Gather Medical Information: If possible, collect information about the person’s medical history, current medications, and allergies to share with emergency responders.
Why Every Second Counts: The Science Behind the Urgency
Understanding the medical urgency helps reinforce why immediate action is so important. When blood flow to the brain is blocked or reduced, brain cells are deprived of oxygen and glucose, which they need to function. Without these essential nutrients, neurons begin to die through a process called ischemic cascade.
Within the first few minutes, affected brain cells enter a state of dysfunction but may still be salvageable. However, as minutes turn into hours, more cells die permanently. The area of dead tissue is called the infarct core, and surrounding it is the penumbra—brain tissue that is injured but potentially salvageable with prompt treatment. The goal of emergency stroke treatment is to save as much of the penumbra as possible.
Modern stroke treatments like mechanical thrombectomy (physically removing a clot) and tPA (dissolving a clot with medication) can dramatically improve outcomes, but only if administered quickly. Studies show that patients who receive tPA within 90 minutes of symptom onset have significantly better outcomes than those treated later.
Expert Stroke Care at Laxmi Hospital Kochi
When it comes to stroke care, having access to a well-equipped, experienced medical facility can make all the difference. Laxmi Hospital Kochi is recognized as a leading healthcare institution in Kerala, offering comprehensive stroke care services with state-of-the-art technology and a dedicated team of neurologists and emergency medicine specialists.
The hospital’s stroke unit is equipped to provide rapid diagnosis and treatment, featuring advanced neuroimaging capabilities including CT and MRI scanners that can quickly determine the type and location of a stroke. This rapid diagnostic capability is crucial for making informed treatment decisions within the critical time window.
Laxmi Hospital Kochi’s multidisciplinary stroke team includes neurologists, neurosurgeons, interventional radiologists, rehabilitation specialists, and specially trained nurses who work together to provide comprehensive care from the moment a stroke patient arrives through their recovery and rehabilitation. The hospital maintains round-the-clock emergency services, ensuring that stroke patients receive immediate attention at any time of day or night.
For the community in Kochi and surrounding areas, Laxmi Hospital serves as an important resource for stroke prevention, education, and treatment. The hospital regularly conducts awareness programs about stroke recognition and prevention, helping to educate the public about risk factors and warning signs.
Risk Factors and Prevention
While knowing how to respond to a stroke is critical, prevention is equally important. Understanding your risk factors can help you take proactive steps to reduce your chances of having a stroke:
Modifiable Risk Factors include high blood pressure (the leading cause of stroke), diabetes, high cholesterol, obesity, physical inactivity, smoking, and excessive alcohol consumption. Many of these can be controlled through lifestyle changes and medication.
Non-Modifiable Risk Factors include age (risk increases with age), family history, race (some ethnic groups have higher risk), and prior stroke or TIA (transient ischemic attack, sometimes called a “mini-stroke”).
The Importance of Acting Even If Symptoms Disappear
One crucial point that cannot be overstated: even if stroke symptoms disappear after a few minutes, you should still seek immediate medical attention. This could indicate a transient ischemic attack (TIA), which is a temporary blockage of blood flow to the brain. TIAs are major warning signs that a full stroke may be imminent—in fact, about one-third of people who experience a TIA will have a stroke within a year if left untreated.
Conclusion: Be Prepared to Save a Life
Stroke is a leading cause of death and disability worldwide, but it is also one of the most treatable medical emergencies when caught early. The first five minutes after symptoms appear are your most powerful opportunity to change the outcome. By learning the FAST signs, knowing additional warning symptoms, and understanding the critical importance of immediate action, you can be prepared to save your own life or the life of someone you love.
Remember, never ignore stroke symptoms, never wait to see if they improve, and never hesitate to call emergency services. When it comes to stroke, every second truly counts. Share this information with your family, friends, and community. The life you save could be your own.
If you’re in the Kochi area and need information about stroke prevention, risk assessment, or treatment options, Laxmi Hospital Kochi stands ready to provide expert care and guidance. Don’t wait until an emergency occurs—be informed, be prepared, and be ready to act when those crucial first five minutes begin.
